My 7th Minute
By Jeffrey Iredell
Introduction
Every 7 minutes, someone in the United States
is diagnosed with lymphoma. That means nearly 80,000 new patients each year
split between the two types of the disease, Hodgkin Lymphoma (appr. 10%) and Non-Hodgkin
Lymphoma (appr. 90%). Although lymphoma
is the most common blood cancer in adults and the third most common cancer
overall in children, lymphoma remains one of the most complex cancer diagnoses
with more than 70 different subtypes of the disease. Currently nearly 800,000 people in the U.S.
are living with or in remission from a form a lymphoma.
Recently, a high school student whose parents work with me on fund raising was asked to do a school project on a type of cancer. He knew of my story and asked if I could help. This is what I put together for him, I hope it helps you as well.
Recently, a high school student whose parents work with me on fund raising was asked to do a school project on a type of cancer. He knew of my story and asked if I could help. This is what I put together for him, I hope it helps you as well.
My 7th minute came up on September 8th,
2011. I was in my car on the way to work
when I felt a small twinge in my back near my shoulder blade. Over the next 36
hours, the pain steadily increased. When
I tried to lay down that night, it felt like someone was stabbing right through
my back. I couldn't catch my breath and
promptly went to the emergency room.
Thankfully, it's only 5 minutes away. After being sedated to relax my breathing and
a chest CT scan, I was diagnosed with a pulmonary embolism (a blood clot in the
lung), unchecked, it would have happily killed me in short order.
Testing
and Diagnosis
 I was admitted and
immediately placed on anti-coagulants and pulmonary monitors. Each of the department doctors were asking
their questions while trying to figure out what had possibly caused the
clot. The last doctor to come in was
the hematologist. He had talked with the
radiologist who had additional findings on the CT scan. They found that my spleen was swollen as were
several on my lymph nodes. He ordered a
full body CT with a contrasting agent to get a better picture of what was going
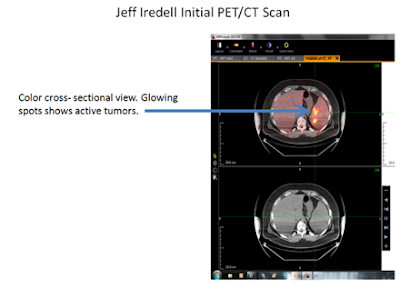
on. The picture below of my scan shows a
few tumors jumping off the page. My
doctor ordered a biopsy of the two on the right side of my abdomen for the next
day.
I was admitted and
immediately placed on anti-coagulants and pulmonary monitors. Each of the department doctors were asking
their questions while trying to figure out what had possibly caused the
clot. The last doctor to come in was
the hematologist. He had talked with the
radiologist who had additional findings on the CT scan. They found that my spleen was swollen as were
several on my lymph nodes. He ordered a
full body CT with a contrasting agent to get a better picture of what was going
on. The picture below of my scan shows a
few tumors jumping off the page. My
doctor ordered a biopsy of the two on the right side of my abdomen for the next
day.As I was being prepped for my biopsy, that was the first time I heard the word, 'lymphoma'. The radiologist stated to me that when he goes in for a biopsy in a lymph node in that area, it's usually lymphoma. I tucked that away in my head to research when I got back to my room. It was also the first time I met 'Sparky', a radiology nurse that I would run across many times over the next several months. We hit it off immediately as we both had the same goofy sense of humor.
When I got back to my room, I
immediately hopped on my computer and found the Lymphoma Research Foundation's
site and the amount of information available was impressive. What I did learn could only be applied to a
point as a specific sub-type had yet to be determined.
So what is lymphoma? In the most general terms, Lymphoma
is a type of blood cancer that occurs when lymphocytes--white blood cells that
help protect the body from infection and disease--begin behaving abnormally.
Abnormal lymphocytes may divide faster than normal cells or they may live
longer than they are supposed to. There
are 3 types of lymphocytes: B-cells, T-cells, and NK cells and each present
their own unique issues. These abnormal
cells are sometimes triggered by an already weakened immune system from other
conditions. A good example of this are
the medications used to treat serious arthritic conditions. The medicines aggressively treat
inflammation, but have the unfortunate effect of weakening the immune
system. For instance, we are all
familiar with all the warnings at the end of drug commercials on
television. One currently running for
psoriatic arthritis drug Enbrel (featuring pro golfer Phil Mickelson as a
patient and spokesperson) states the following as part of the warnings and can
also be found right on the website (www.enbrel.com), "There
have been some cases of unusual cancers reported in children and teenage
patients who started using tumor necrosis factor (TNF) blockers before 18 years
of age. Also, for children, teenagers, and adults taking TNF blockers,
including ENBREL, the chances of getting lymphoma or other cancers may
increase. Patients with RA or psoriasis may be more likely to get
lymphoma". Now to
be sure, that doesn't mean it's likely that
you will get lymphoma, it just
increases the risk. Needless to say, if
I ever get a serious arthritic condition, these types of drugs are off-limits
to me.
Lymphoma may develop
in many parts of the body, including the lymph nodes, spleen, bone marrow,
blood or other organs. My initial scan certainly fit the description.
The real issue with lymphoma is that until
serious symptoms present, it often goes unnoticed or misdiagnosed, usually as
an infection. I can't tell you how many
of my friends in the lymphoma community were first prescribed a couple of
rounds of antibiotics for swollen lymph nodes in the neck, which is usually a
symptom of an advanced condition. Some
possible indicating symptoms include fatigue, fever, unexplained weight loss,
drenching night sweats, chills, labored breathing, and itching. You can see how it's easily overlooked as there
are hundreds of other conditions that share some or many of these symptoms.
There is no blood test for diagnosis and it
is usually caught as a secondary finding, much like my situation. The only sure way to diagnose it is through a
biopsy. Once a person achieves remission, we do keep an eye on one possible
blood indicator- LDH or Lactic acid Dehyrogenase, an enzyme that helps produce
energy. An elevated level raises a flag, but it is only a diagnostic tool that
leads to further testing for a diagnosis.
A day or so later, initial results came back
from the local pathologist- initial findings were of Follicular non-Hodgkin
lymphoma, an indolent or 'slow-growing' form.
My slides were sent off for a second opinion (thankfully so, but more on
that coming up).
Follicular forms are difficult to treat and
fairly uncommon in people of my age (44 at the time) or younger. Most therapies for cancer treatments target
rapidly dividing cells and this form is not.
It is also an incurable form, but today's therapies can place it in long
periods of remission, currently estimated at 15-18 years now. Given the average age of diagnosis for this
form, most people diagnosed with this form live a full active life and pass
away from old age or other disease long before the cancer overcomes them.
We started to schedule a battery of
pre-treatment testing and procedures we could do while waiting for the second
opinion on my slides.
A
couple days later I was released from the hospital on blood thinners. It’s crazy to think that I survived a blood
clot just to face a cancer diagnosis.
When it rains, it pours.
First
up was a Positron Emission Tomography scan or PET scan. This is similar to a CT
scan, but is specifically designed to show metabolic activity in cells whereas
a CT is great for defining the size and shape of the anomaly. They usually take a CT shot at the same time.
The PET scan process begins by fasting after
midnight before the test. When you
arrive, you first have a blood sugar test to make sure you are in a normal
range. The next step is why: Through a
vein, you are then injected with a radioactive glucose with a very short
half-life. You typically wait 30-45
minutes to allow the body organs and cells to absorb this tracer before being
scanned. My particular center keeps you
in a quiet room with the lights off, no external stimuli, cells phones, music,
nothing. I usually just catch a
cat-nap. Some centers allow music, but
the idea is to quiet as much of the body as possible to really see which cells
are over active as they more readily absorb the glucose for energy.
The scan is much longer than a CT, you place
your head in a cradle to keep it still as well as a large body strap to try and
keep you in place. You don't realize how
hard it is to stay still until you need to do it. The machine is very similar to the CT, but it
can only scan a portion of you at a time. They scan will start with the table
being still and then move you every couple of minutes through the scan area
until the scan is complete. Now as
someone who is a bit taller at 6'1", my scan takes an excruciating 28
minutes. My arms almost always fall
asleep after about 5 minutes. You start
to make up games in your head to pass the time, whether counting the seconds
down to see if you can time the move to thinking the alphabet backwards and
more.
Results get read by the radiologist and are
available a couple days later for me, either through meeting with my doctor or,
as I now usually do, getting a CD copy and looking at it myself. Below is the CT portion of my PET scan. You can see the dark spots all over my body,
some lighter than others. I had
lesions/tumors on my spleen, lymph nodes, rib cage, humorous on my left arm,
and disturbingly one of my vertebrae.
On the PET scan, generally
any activity over a factor of 4 in an area is cause for concern (with the
exception of the brain, heart, kidneys, and bladder as the first two naturally
use and absorb energy and the other two are the final filters the tracer passes
through to pass). The areas will light
up like a light bulb.
In short, I was already a stage 4 lymphoma
patient and didn't know it until I developed that blood clot. While stage 4 sounds serious, and it is, it's
not the same as most other cancers. Most
other cancers it indicates a low chance of survival. With lymphoma's, while lowering the odds
somewhat, it is more used to indicate what in the body has been affected, the
Ann Arbor staging system is as follows:
Stage I
Either of the
following means the disease is stage I:
§
The lymphoma is in only 1 lymph
node area or lymphoid organ such as the thymus (I).
§
The cancer is found only in 1
area of a single organ outside of the lymph system (IE).
Stage II
Either of the
following means the disease is stage II:
§
The lymphoma is in 2 or more
groups of lymph nodes on the same side of (above or below) the diaphragm (the
thin band of muscle that separates the chest and abdomen). For example, this
might include nodes in the underarm and neck area but not the combination of
underarm and groin nodes (II).
§
The lymphoma extends from a
single group of lymph node(s) into a nearby organ (IIE). It may also affect
other groups of lymph nodes on the same side of the diaphragm.
Stage III
Either of the
following means the disease is stage III:
§
The lymphoma is found in lymph
node areas on both sides of (above and below) the diaphragm.
§
The cancer may also have spread
into an area or organ next to the lymph nodes (IIIE), into the spleen (IIIS),
or both (IIISE).
Stage IV
Either of the
following means the disease is stage IV:
§
The lymphoma has spread outside
the lymph system into an organ that is not right next to an involved node.
§
The lymphoma has spread to the
bone marrow, liver, brain or spinal cord, or the pleura (thin lining of the
lungs)
Shortly after my scan, the second look at the
slides came back from Johns Hopkins, they disagreed with the initial findings,
they identified it as Diffuse Large B-cell non-Hodgkin lymphoma (often
shortened to DLBC), it’s the most common form of lymphoma, although I did also
have some of the previously mentioned T-Cells involved as well. This is a different animal that the previous
findings, if true, this is an aggressive form that will require quick movement
into treatment, so we accelerated the testing while we sent the slides to a third
site at Fox Chase in Philadelphia for a look-see.
Meanwhile, Testing continued over the next
couple of days. I had a muga scan (a test using a radioactive tracer (called a radionuclide) and
a special camera to take pictures of your heart as it pumps blood. The test
measures how well your heart pumps with every heartbeat). This is crucial to make sure you can handle
the treatment as the chemo regimen can damage the heart.
I
next had an MRI (Magnetic Resonance Imaging) on my spine to try and determine
how far it had advanced in my vertebrae. The results were inconclusive as to
whether it had gotten through to the spinal fluid. That led to a lumbar puncture (better known
as a spinal tap) to get some spinal fluid as test it for cancer cells. The fluid came back negative.
Lastly
and most dreaded-the bone marrow biopsy.
This test involves you either lying on your side in a tight fetal
position or lying on your belly with a pillow under the hips. Next, the area on the back of the hip called
the iliac crest is marked and the surrounding soft tissue is numbed with
lidocaine. Next, a guide tube is
inserted down to the hip bone. This is
all relatively painless at this point if you are breathing regularly and trying
to stay relaxed, a lesson I learned the hard way. Next, what can best be described as a
corkscrew, is inserted into the guide tube and a core is started through the
bone to access the marrow. While this
too sounds painful, bone doesn't have pain receptors, but once the core is into
the marrow, there is a bit of pain. The
coring tool is removed and what happens next is 5 seconds of intense pain as
some of the marrow is sucked out for testing along with a small piece of the
bone itself and then it's over. You are
bandaged up and kept for 30 minutes to make sure there is no excessive
bleeding. The anticipation of the pain
is often worse than the pain itself.
Having
had both versions at this point, I can tell you I definitely prefer lying on my
belly, it's easier to relax and continue breathing easy. Moreover, the Physicians Assistants at Fox
Chase are well practiced and keep you talking about pleasant things the whole
time to keep your mind off of it.
Anyway, the testing came back positive for marrow involvement, so great,
just another strike. That said, I never
had a 'why me?' moment. From the get-go
I was determined to win and no matter what was getting thrown at me, I stayed
upbeat. I truly believe this attitude
has gotten me to where I am today.
After reviewing all the data, my doctor suggested a course of chemotherapy
called R-CHOP. I would be infused every
3 weeks for 6 to 8 rounds depending on progress. Each of the letters represents one of the
five drugs in the therapy. R-Rituxamab, C-Cyclophosphamide, H-Doxorubicin
Hydrochloride, O- Oncovin (also known as Vincristine), and P- Prednisone.
He
also suggested 4 rounds of intrathecal chemo (spinal tap performed with a
little fluid drawn out and replaced with chemo) with Methotrexate as a
preventative measure to protect my spinal fluid.
At my doctor’s suggestion, I had a second opinion with Dr. Mitchell
Smith at Fox Chase Cancer Center. As Fox
Chase is a teaching hospital, I would also be meeting with an underling on a
fellowship grant. The doctor confirmed
the diagnosis and agreed on the suggested treatment plan.
He then started explaining the IPI or International Prognostic Index,
basically your odds of surviving 5 years past treatment without a recurrence of
the disease. At this moment, in my
typical coping manner of mocking my disease I went Han Solo on him, “Never tell
me the odds”. In short, it didn’t matter, I wasn’t going to be a statistic, I
was simply going to survive. The other
reason I took it with a grain of salt is that the index was created in 1993 (18
years before my diagnosis) and based on a slightly different treatment, it had
not yet had enough data to include the addition of the Rituximab in my
regimen. Anyway, he gave me a 51% chance
of staying in complete remission. Recently, an updated index has become
available called the R-IPI to include the addition of Rituximab to the
mix. The results of adding the
Rituximab are astounding, I jumped from 51% to 79% (www.qxmd.com) on the new index. As we find out a little later, it didn’t
matter as I still fell into the 21% that relapse.
Treatment
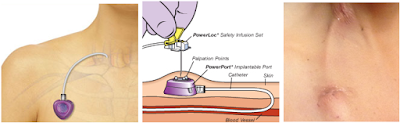
In
mid-October, I had a Power Port© inserted in my chest. As shown below, it is a
heart-shaped silicon reservoir with a catheter that is inserted directly into
the jugular vein. It is used to deliver
chemotherapy to cancer patients who must undergo treatment
frequently. Chemotherapy is often toxic, and can damage skin and muscle tissue,
and therefore should not be delivered through these tissues. Another drawback
to using traditional IV’s is overuse will ‘collapse’ a vein over time and make
it inaccessible. Ports provide a solution, delivering drugs quickly and
efficiently through the entire body via the circulatory system. It can also be
used to draw blood tests, inject CT contrast and other uses as well. Once the insertion area heals, it’s almost
unnoticeable to the patient.
I started my
first chemo treatment on October 31st, 2011. Day 1 was the Rituximab only. It’s a 6 hour infusion and patient often
experience an allergic reaction the first time they receive it. They first pre-treat you with Benadryl© and
an anti-nausea medication before starting.
They slowly increase the infusion rate to be better able handle the
allergic reactions that may occur. Most
people simply develop hives or flushing and simply need the flow to temporarily
stop, take some more Benadryl and continue on.
Nope, not me, I got one of the more uncommon reactions.
I developed what
is called ‘Rigors Syndrome’. Essentially
your body begins to feel colder (although your actual body temperature is still
normal) and no matter how many blankets you throw on you, the still feel cold
and shake uncontrollably. The only way
to stop the reaction is to stop the infusion and get injected with a
significant dose of Demerol©, typically used to relive moderate to severe pain,
but has this application as well.
Needless to say, it immediately calmed me down. After 30 minutes off the infusion, we
restarted and finished without further complication.
The next day I
returned to have 3 of the other drugs, the C-Cyclophosphamide,
H-Doxorubicin Hydrochloride, and O- Oncovin. I was sent home around mid-day
with several prescriptions. One for Uric
acid build up, my P (Prednisone), and
two for possible nausea. I spent most of
the time in the infusion room reading, napping, or harassing the nurses.
Let’s
talk about the nausea for a second.
Don’t let the old movies or TV shows skew your thinking about nausea
from chemotherapy. In all of those older
shows, they depict cancer patients constantly vomiting. Maybe I am of sturdier stuff, but I didn’t
get sick in that way once during my entire treatment, the anti-nausea drugs do
their job very well and have come a long way since the 1970’s and 80’s.
That
doesn’t mean I didn’t experience side effects though. The two big ones were fatigue and loss of
appetite for me. I did find a way to
cope with each. For the fatigue, just
getting on my treadmill for 30 minutes or so helped keep my energy level up
enough to make it almost through a normal day.
The appetite was a bit trickier, but that’s one of the things Prednisone
helps with, many people on Prednisone during treatment actually gain weight and not lose it.
Unfortunately, it also has the effect of restlessness and not allowing me to
sleep for the 5 days I was on it each round. That was helped by getting
prescribed Ambien©.
On
the third day I was required to go back in for a shot called Neulasta©. This is essentially a drug designed to help
boost white blood cell production.
Remember those B, T, and NK cells we talked about earlier? Well chemo kills them off fairly effectively
as it doesn’t discriminate between healthy and mutated cells. As such, about 5 days after treatment, you
are at a high-risk for infection since so many of the existing healthy cells
have been destroyed. This is why you
have 3 weeks in between, to allow your body to recover. The good news is that’s
why chemo works. Healthy cells have the ability to repair themselves through
the rest of the body chemistry while the cancer cells don’t.
Neulasta does have one possible nasty side effect, severe bone and joint
pain. I experienced this about 1 ½ hours
after my shot. As I was walking out of
Target my hip joints literally locked in place from a sudden and excruciating
pain. I hobbled to my car and sate there
for about 15 minutes until I could handle it well enough to drive. In spite of having some pain medication to
take, I still had some discomfort for a couple of days.
On the off week I had to have blood work done and mentioned this to the
nurse. She mentioned some people have
luck taking Claritan© before and after the Neualsta as an ingredient helps
counteract the effect. So I tried it the
next time around and it worked for me.
So that was my life for the next 6 months. I worked when I could at the office and from
home when I couldn’t. My employer was
very understanding and worked with me throughout. I really can’t thank them enough.
After the 2nd treatment we performed a CT scan to check early
progress and things were going swimmingly.
The tumors had begun to shrink significantly.
After
my 3rd or 4th treatment, I knew I was doing well, I could
feel it. I wanted to find a way to get
involved and give back to the lymphoma community. My sister discovered the Lymphoma Research
Foundation (LRF) was hosting a 5k charity walk in the fall. We immediately started a team knowing I would
be out of treatment and well on the mend by then.
After the 4th treatment the plan called for the round of
intrathecal chemo to begin. As mine was
only for 4 rounds, I did not need to have an Ommaya inserted, basically a chemo
port placed in the skull. This chemo needs to done this way as most chemotherapies
cannot penetrate what they call the ‘blood-brain barrier’. It’s the body’s natural defense to keep as
many foreign objects out of the cerebral-spinal fluid as possible.
By starting the intrathecal portion on my
5th round, we had already determined to go for 8 rounds instead of
the hoped for 6. Of course I was a bit
disappointed to need the extra treatment, but better safe than sorry. After my
6th round of treatment I had another PET scan. The results came back pristine, NED or ‘No
Evidence of Disease’. I still had a
little way to go, but the light was getting much brighter at the end of the
tunnel.
My final chemotherapy treatment was on April 2, 2012. No words suffice to describe the sense of
pride on my victory. That said, I still needed to clear 2 more hurdles before
being officially declared in remission.
I still needed to have a post-treatment bone marrow biopsy (BMB) and
another PET scan 6 weeks after treatment ended.
Survivorship
Through it all, my sister acted as my caregiver, she was the best. Rides, house cleaning, general support, I
couldn’t have done it without her. I
tried to remain as independent as possible, but really had to lean on her for
some things. I think that was a key
though, trying to keep as normal a life as possible, it made my adjustment from
patient to survivor easier than some. I
didn’t have to reintegrate back into life.
People often ask how I coped with everything throughout it all. First, I stayed positive, no set back was
going to bring me down. Secondly, I
found a support board on Facebook run by a Hodgkin lymphoma survivor called,
‘The Lymphoma Club’. Being able to bounce
things off of other patients really helped gain perspective and gather coping
ideas. Some I liked, some not. That’s one piece of advice I think everyone
can take away, not everybody copes with events in their life the same way. Listen to all and take what works for you,
don’t believe those that tell you it’s the only way.
I
also found something else on that page, women are far more likely to seek
support and also offer support whereas men generally internalize in some sort
of need for machismo in a time of need.
I actually had the page moderator post a survey for me on various
demographics and 94% of the respondents were female and to no one’s surprise,
tended to be a younger demographic in the Facebook world.
The
weekend following my final chemotherapy, I went out to watch my softball team
play our season opener against a team also sponsored by our company so it was a
bit of a rivalry game. We only had the
minimum 10 players show up and in the 4th inning, one of them got
injured and could not continue, I was pressed into service. I hadn’t realized how much my body had been
affected by the relative inactivity from my treatment, sure I was on the
treadmill almost daily, but hadn’t understood my muscle atrophy well at all.
I
came to bat in the 5th inning and hit a line drive to left
field. I never saw the ball land. I took one step to run to first and my back
toe caught and down I went. I landed
awkwardly with my right arm tucked under my ribs and immediately felt a searing
pain in my rib cage. If I didn’t crack a
couple of ribs, I sure as hell badly bruised them. I did get right back up and start to jog to
first and then I realized the issue. I
literally had to learn how to run again and strengthen those muscles. I felt my knees try to hyper-extend with each
step. In my mind I looked and felt like a baby giraffe trying to walk or run
for the first time. I stuck it out and
even hit the walk-off single to win the game, but made sure to take my time
going down to first. I was sore for
about a week.
The following week I had my BMB and waited for results. In the meantime, I had pretty much returned
to work full time. About a week later I
was at home playing dominoes with my sister and friend and received a phone
call from my nurse. The BMB results had
come back negative. I hung up and gave a
yawp. My sister asked and I told her to sit down and she had fear in her eyes,
right up until I told her the results.
She cried with joy while I danced a jig.
I felt the need to celebrate. Now
keep in mind that I hadn’t had an alcoholic drink in over 7 months. One shot
and one beer later I was quite loopy.
Any tolerance I had was long gone and that’s not a bad thing.
4
weeks later I had my PET scan. We wait
that long after treatment to avoid any false-positives. That scan came back clear and life was back
in full-time mode. I planned a walk team
fund raiser we held at my house over July 4th weekend and we raised
over $4,500 that first year.
The walk was in late September and things were going well. What a great experience, bonding with other
survivors, just a look and we knew what each other had been through. I made
some lifelong friends that day. The
local LRF leadership made sure to meet each survivor and really made us feel
welcome. I was so impressed, I signed up
that day for the following year walk committee.
The holidays came and went with a clear PET scan in December. In late January the walk committee got
together for the first time and shared some drinks, food, stories, and
planning. The next couple of months
brought conference calls and I guess my enthusiasm came through the phone as
the chapter president asked to speak with me alone. The chapter positions are volunteer positions,
we work around our normal lives. His
life was busy with a wife, two kids, and his full-time and part-time jobs, he
didn’t have the time to fully dedicate like he once did. He gave me a sales pitch on becoming
co-president with him and becoming more involved. He finished with, “…and this is where you say
no”.
Except that I didn’t. I happily
said yes. My sister remarked that I
acted like it what was I was meant to do.
Looking back I realize it wasn’t the position itself, it was the ability
to be able to reach out to people in need of guidance, help, and general
support. Whether it’s pointing them in
the right direction for information, offering them coping advice, or providing
inspiration, it’s completely rewarding.
I remarked at the time that I took far more lymphoma than it had ever
taken from me.
Over the next 2 years I attended LRF
sponsored events in both a patient and leadership role. Walks, Ask the Doctor programs, leadership
meetings, and daylong workshops. I had moved on from PET scans to CT scans
every 6 months along with blood tests and doctors appointments. Along the way,
we reorganized to a regional council model and became the vice-chair of the
Northeast Region. Then, in late
November of 2014, on what was to be my final follow up CT scan, we had a blip
on radar. It was a crappy Christmas.
Relapse
The CT had shown slight growth in a lymph
node, the same one biopsied the first time around. My doctor suggested a PET scan for shortly
after the holidays. In late January we had
the scan and sure enough, that node lit up like a light bulb and 3 others also
had indications of active cancer cells.
The 4-1 odds against me having a relapse had failed me. The good news is that it was caught very
early, the bad news is that I would need to undergo treatment again and it
would be different as this was a relapse.
Again I stayed upbeat, but my confidence was a little shaken, but had
faith in my doctors.
I was referred once again to Fox Chase and
Dr. Henry Fung, a blood cancer specialist.
The first challenge we had was to make sure it was the same type of
lymphoma, remember there are 70 varieties, give or take. My active node was tucked right behind my
aorta (the main artery from the heart) in my belly. He had consulted the radiology team an only 1
doctor of 9 thought they could get at it without damaging the aorta and even
then it would have been an unreliable fine-needle aspiration.
He next suggested an alternative possibility,
a bone marrow biopsy (BMB) in thoughts that some of the cells had infiltrated
that tissue. I groaned having already
expressed my displeasure with them, but I agreed. This was my health after all. The BMB results came back negative.
He consulted with the rest of his team at that
week’s meeting to discuss the proper course of action. The recommendation- 2 rounds of c different
chemo followed by a stem-cell transplant. My heart sank.
Chemotherapy
part 2
I was immediately scheduled to have my power
port reinserted and start chemo the day following. This chemo would be a little harsher so we
could quickly get me in remission to harvest my cells for the transplant, more
on that later.
This chemo regimen was abbreviated as RICE
which was again, the four drugs associated with the letters. R-Ritixumab,
I-Ifosfamide, C-Carboplatin, and E-Etoposide.
The biggest side effect comes from the Ifosfamide, it causes bleeding to
occur in the bladder. The drug is given
over a 24 hours along with a counter-agent called Mesna. The Mesna runs at the same time and for
another 6 hours after the Ifosfamide run is complete. The hospital tests your urine every 6 hours
for traces of blood, so 2 overnight stays are required. I am then released after a shot of the
previously discussed Neulasta© to boost cell count. The two rounds were 2 ½ weeks apart.
While this was going on, my sister and I
scrambled with preparations for the Stem-Cell Transplant (SCT), also known as a
bone marrow transplant. We had to meet
with a social worker to make sure my head (and hers) were in the right
place. Insurance pre-approvals, living
will, advanced directives, orientation and a slew of tests. Pulmonary function,
electrocardiogram, EKG, x-rays, etc.
After the second round of chemo, a PET scan
showed I was in good enough condition to proceed ahead with the SCT process. The doctor gave me an 80% chance of success.
Stem Cell
Transplant
Using my doctors example, think of things
this way: treating a cancer with chemotherapy is like using a machine gun, it’s
an effective killing agent, but may miss here and there. Using the transplant as the secondary option
is like using a nuclear bomb-blow everything up and rebuild again.
There are two types of transplants for blood
cancer patients: Autologous or using the patient’s own cells and Allogeneic -using
a donors cells. Each has its advantages,
but I was targeted for an Autologous transplant. A summary is extracting healthy stem cells from my marrow, blowing up my existing immune system and along with it any
remaining cancer cells, reintroducing my irradiated stem cells and having my
immune system start anew. It’s over-simplified, but if you don’t want the
specifics, you can skip ahead.
The first step was to have a triple lumen line (also known as a Hickman line) inserted into my chest opposite my current chemo port. This central line catheter in the chest allows for multiple actions at once.
Next, I had to give myself 2 injections twice
a day of Neupogen©, a daily version of the Neulasta. I had to do this for 4 days to really build
up cell count to a ridiculously high number in preparation for my stem cell
harvesting. On the 4th evening I was given a drug called Plerixifor and a high dose of Immodium. As
stem cells release very slowly from the marrow, the Plerixifor enables a high
volume to release at once so we don’t need to actually drill into my bones and
suck them from the marrow. The Immodium
was to constipate me as I would not be able to stop the machine to go to the
bathroom once we began.
The apheresis machine hooks up to two of the three lumen lines. One is used for access, the other for return (figure below).
In my case,
they were separating out stem cells. At
the end of the day these were counted in a lab to make sure enough had been
harvested for the transplant, if not, back at it the next day. I needed at least 2.5 million (that’s right,
million, they are small…). The first day
yielded ‘only’ 1.8 million so we repeated the next day and got another 800,000
to finish the cycle. The cells are
irradiated (to kill all disease that may be present) and frozen for use later.
Two days later, on May 22nd, I was
admitted for the long haul, at least 15 days in the hospital, maybe up to a
month. That morning as my sister was
driving us there, I finally broke down in fear.
I didn’t cry, but everything I had been internalizing came out. It was much needed, confronted the fear and
moved on the next step. The admitting
nurse made it easy as it could be, keeping us laughing and relaxing. Then reality, okay, get your room in order, order
lunch and dinner, your first chemo starts around 6 PM tonight.
The first six days would be high dose
chemotherapy, designed to eliminate my existing immune system. It consists of 4 drugs and is titled
BEAM. B- BiCNU (better known as
carmustine), E-Etoposide (again), A-Ara C (better known as Cytaribine), and
M-Melphalan. The best way to describe
the side effects was getting the worst flu you can imagine. While my nausea was pretty well kept in
check, the GI tract issues sucked. And
that is my one best piece of advice, be sure to bring you own, favorite brand
of toilet paper with you, and lots of it.
The hospital sandpaper would have killed me.
Mostly, I was bored. I came prepared, but how many movies can you
watch, laps can you walk, books can be read, and internet be cruised while
you’re fighting for your life? Most of
my entertainment came from joking with the nurses and the daily doctor visits.
On the seventh day, my stem cells were
reintroduced to my body. I shook their
hand and…..okay, not really. My frozen
stem cells were slowly thawed out and injected slowly into my blood
stream. It’s pretty anti-climatic. 30 minutes later, it was down, my new
birthday was May 29th, 2015.
Post-Transplant
I wasn’t home free yet, not even close. My cell count had yet to bottom out and the
new cells take over. Three key stem
cells numbers are watched- Hemoglobin, Platelets, and Absolute Neutrophils
Count (white cells ANC). If either of
the first two got too low, I would have either receive a pint of blood or
platelets, whichever was needed at the time.
The ANC however was the key. I
was at a high risk for infection until they got to a safe level. They expect you to spike a fever at some
point, and boy did I. I hit almost 104
and had very low blood pressure so I had to spend a night in the ICU until the
antibiotics stabilized me.
On day plus 4 I hit the zero ANC mark, which
is expected, now we had to wait for the number to start creeping up. I continued to feel crappy, but that’s
expected. Sleeping was difficult. They pump full of fluids so you don’t
dehydrate, so bathroom runs every hour, uncomfortable beds, and your blood work
every morning between 4:30 and 5 am. I
do have to say, the food was quite good though.
On day plus 7, my ANC ticked up to 0.1, not a
huge number, but we were moving! It progressed over the next few days and on
day plus 12- June 10th, I was released from the hospital. God it felt good to breather fresh air!
I still needed to remain at home and
semi-isolated for a long time. I had
diet restrictions, cleaning restrictions, and took time regaining my
strength. I returned to work on July 27th. In September I had my follow up PET scan and
BMB, both were clear.
Life was slowly returning to normal. In November I started with my re-immunization
schedule. If you recall, my immune
system was blown up so I have to get all of my childhood vaccinations again. I returned to golfing and helping out at LRF
functions.
April 23rd I had my 1-year PET
scan. I couldn’t wait to meet my doctor on it, I took a look at the CD copy and
it’s clear. (Doctor confirmed the
following week) I have my 1st birthday as a new man coming up in 2
days and I am thrilled as can be. Go
me.
That was the longest 7 minutes ever.